Global Health
History | Philosophy of Training | Curriculum Topics | Global Health Experience
Underserved health
Continuity Sites | Addiction Medicine | Advocacy | Community Engagement | Climate Change
Our history
Our program is nationally known for its longitudinal training in Global Health. A pioneer in the Global Health field since 1991, we have a long-standing commitment to train and inspire adaptable physicians to lead and serve in healthcare for underserved and vulnerable populations both in the United States and internationally.
Our curriculum reflects this commitment, featuring integrated global health rotations, monthly global health conferences, diverse scholarship opportunities, and strong community medicine experiences.
Our residents are encouraged, but not required, to participate in our global health experiences. Residents enjoy fully funded trips during their first two years and $2000 towards a third-year experience. Our dedicated faculty members have broad experience as long-and short-term medical providers in Honduras, Cambodia, Haiti, Cameroon, Kenya, Tanzania, and Armenia.
Our global health philosophy
We train family physicians to work with vulnerable populations: whether they live across the world or in our own backyard. Vulnerable populations are those patients who are economically, politically, culturally, ethnically, geographically or in any way marginalized. We view Global Health as a multidisciplinary approach to health that takes into account all the determinants of health- social, environmental and physical.
Our curriculum includes speakers from many disciplines: anthropology, nursing, dentistry, pediatrics, public health, and psychiatry. This framework allows us to address issues which face vulnerable populations everywhere, and prepares the physician to address these issues, in whatever practice setting they find themselves.
A few current curriculum topics include:
Social determinants of health
Public policy, advocacy, and leadership
Community and population health
Cultural competence
Disaster relief and health care systems
Models of medical care
Nutrition, child health, education
Women's health in foreign countries
Infectious disease
Care of LGBTQIA+ adult patients in a global setting
Chronic disease management
Mental health
The current Global Health experience
Our current partnership is with Wuqu' Kawoq: Maya Health Alliance, a non-profit organization based in Guatemala. This organization provides care to rural, indigenous Mayan communities in their native languages. Wuku' Kawoq's nurses and physicians collaborate with the Guatemalan healthcare system by integrating with local health promoters to expand on preexisting health resources and infrastructure.
Our residency program has been partnered with this organization since 2015 to increase their medical services offered throughout the year, although care continues to be provided primarily by medical workers in-country, even in our program's absence. In addition to direct patient care, the residency has worked with the organization on a variety of quality improvement and public health projects, including women's health, chronic disease management, and mental health.
We are currently working with the organization to integrate telehealth visits into our collaboration and may soon be able to provide health care remotely for some of Wuqu’ Kawoq’s communities.
Check out the TCH/UCFM Global Health Facebook Page!
Underserved care in our own community
Aside from learning to care for vulnerable populations in international resource-limited settings, you will have long term continuity clinic sites within the Greater Cincinnati community.
In addition to the Family Medicine Center where residents carry a patient panel reflective of our city demographics, we receive extensive training in cultural competency, the impact of the history of our city, and social determinants of health. We have an expanded reach through our continuity sites, where each resident will practice medicine longitudinally at one of the following:
Crossroad Health Center: An urban, faith-based Federally Qualified Health Center located in Over-the-Rhine that serves many inner city and underserved patients.
NeighborHub Health: An urban clinic in the Over-the-Rhine neighborhood serving mostly patients experiencing homelessness, and those with mental illness. Works with a lot of patients who are transitioning out of the prison system and also provides care in addiction medicine.
Good Samaritan Free Clinic: A philanthropically supported free clinic in the Price Hill neighborhood that focuses on providing comprehensive care to uninsured adults, including a large immigrant and hispanic population.
Additionally all residents will have opportunities to spend time at the Belterra's Race Track Clinic: A clinic for mostly migrant workers at a local horse race track.
ADVOCACY
Advocacy is our response to health inequities and can occur at all levels. Working one-on-one with a patient to get a prior authorization for medication is advocacy. Quality improvement to address the systems in our office is advocacy. Educating ourselves and others is advocacy. Working in hospital communities to change policy is advocacy.
Our advocacy curriculum is woven throughout training. Supplemental opportunities to deepen skills are available through electives. Extra-curricular projects and teamwork are easy to join.
Our residents are bonded by our dedication to social justice, and you can often find us collaborating on advocacy work over a meal or a drink during our free time.
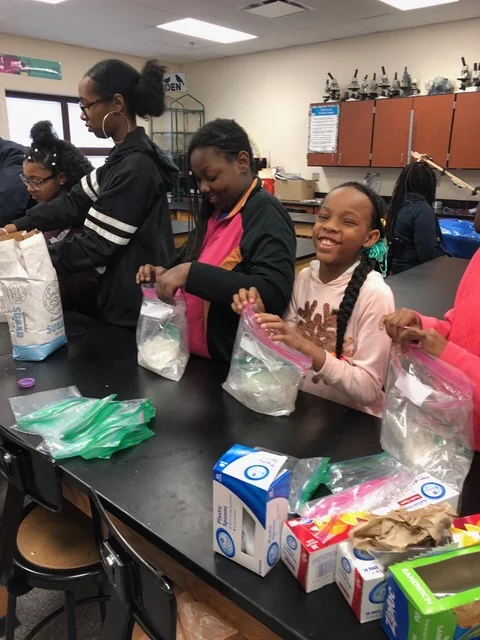
community engagement
Another exciting recent addition to our program is a partnership with Walnut Hills, an urban neighborhood in close proximity to the hospital. The Walnut Hills Committee is dedicated to creating opportunities for residents, faculty, and staff to further engage and serve the community outside of the clinic. Walnut Hills is one of the oldest neighborhoods in Cincinnati, rich in history and culture, and home to many of the patients we serve at the Family Medicine Center. In the Walnut Hills Committee, we are fortunate to partner with other local organizations dedicated to promoting education, safety, health equity, and well-being for members of the neighborhood, such as the Walnut Hills Redevelopment Fund and Center for Closing the Health Gap. Past collaborations with these organizations include healthy food access through volunteering at local community gardens and educational outreach through our Road to Medicine program. Over the course of this next year, we also plan to provide cooking classes (either remotely or in-person, depending on COVID-19 risk) for families in the Walnut Hills community. We are always looking to establish new connections in the community and opportunities to empower the neighborhood.
Addiction medicine
We have a partnership with the Greater Cincinnati Behavioral Health to provide opportunities for residents to gain hands on experience in medication assisted treatment (MAT). We are supported by our UC psychiatry colleagues and are working on expanding the curriculum.
CLIMATE CHANGE AND VULNERABLE COMMUNITIES
The Green Committee is a relatively new resident-run committee aiming to address sustainability issues, both in the Christ Hospital system and in our communities. Extreme weather events overlap with adverse health effects, political instability, poverty, displacement, poverty, food insecurity, and problems related to unreliable infrastructure the world over, and our residency hopes to work with the local healthcare systems to both improve sustainability efforts and foster resiliency in local communities and the broader political and public service infrastructure. Look for more info on projects led by the Green Committee coming soon!